Good News: The US Maternal Death Rate Is Stable, Not Sky Rocketing, As Reported
Philadelphia | March 13, 2024
New research in the American Journal of Obstetrics & Gynecology uncovers data misclassification and refutes the widely accepted view that maternal mortality rates in the US have risen dramatically
A new study(opens in new tab/window) published in the American Journal of Obstetrics & Gynecology(opens in new tab/window), published by Elsevier, challenges the prevailing view on the maternal death rate in the United States. The findings show that the rates of maternal death were stable between 1999-2002 and 2018-2021, instead of the dramatic upward trends previously reported by the National Vital Statistics System (NVSS), Centers for Disease Control and Prevention (CDC). Additionally, the study indicates that direct obstetric causes of death declined over the last 20 years.
To determine whether the reported maternal death rates are accurate, a team of researchers took a deep dive into the underlying data and looked at the factors driving the increase, namely, changes in obstetric factors, maternal chronic conditions, and surveillance issues (i.e., changes in data collection methods). Maternal deaths refer to those occurring during pregnancy, childbirth, or the postpartum period from conditions directly related to pregnancy or those exacerbated by pregnancy and birth (accidental and incidental deaths in pregnancy are not included in the maternal death definition).
Lead author K.S. Joseph, MD, PhD, Department of Obstetrics and Gynaecology, University of British Columbia and the Children’s and Women’s Hospital and Health Centre of British Columbia; and School of Population and Public Health, University of British Columbia, said “Our study showed that maternal mortality rates were low and stable between 1999–2002 and 2018–2021, which is very different from the high rates and dramatic increases reported by the NVSS in recent years. We found that exclusive reliance on the pregnancy checkbox on death certificates, without corroboration from the cause-of-death information, led to an overestimation of maternal mortality rates by the NVSS in 2018–2021.”
Researchers examined all deaths in the US between 1999 and 2021 using an approach that enables greater accuracy in how maternal deaths are identified and classified in the mortality database. The study uncovered several indications that the pregnancy checkbox was responsible for misclassifying nonmaternal and incidental deaths in pregnancy as maternal deaths. These included a 46-fold increase in maternal deaths among women with malignant neoplasms (which likely represent incidental deaths in pregnancy and not maternal deaths). Also, a substantially higher proportion of maternal deaths identified by the pregnancy checkbox had a single entry in the cause-of-death section, which requires a listing of all the immediate, intermediate, contributory, and underlying causes of death (thus suggesting a less thorough approach to death certification).
Although the pregnancy checkbox was introduced on death certificates in 2003 to improve identification of maternal death, its use between 2003 and 2017 was associated with some substantial errors. A detailed investigation by the National Center for Health Statistics (NCHS), CDC showed that the checkbox was erroneously ticked in many cases, leading to misclassification and overestimation of maternal death. For example, hundreds of decedents, 70 years of age and older (including 147 women aged 85 years and older in 2013), were certified as pregnant at the time of death or in the year prior. The NCHS concluded that the entire increase in maternal mortality in the US between 2003 and 2017 was due to the pregnancy checkbox. In response, NCHS made specific changes regarding pregnancy checkbox use for deaths from 2018 onwards but NVSS reports show that maternal mortality rates have continued to increase (nearly doubling from 2018 to 2021).
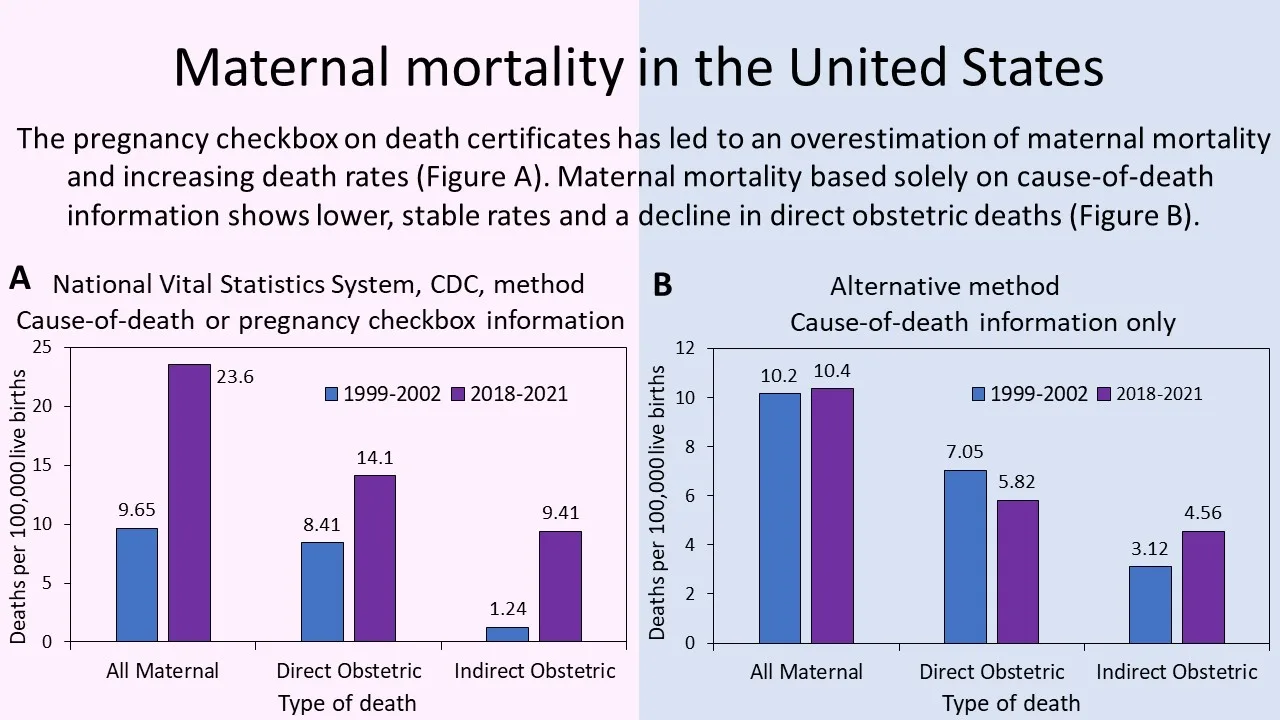
Caption: Maternal mortality in the United States. The pregnancy checkbox on death certificates has led to an overestimation of maternal mortality and increasing death rates (Figure A). Maternal mortality based solely on cause-of-death information shows lower, stable rates and a decline in direct obstetric deaths (Figure B) (Credit: Joseph KS, Lisonkova S, Boutin A, et al. Maternal mortality in the United States: are the high and rising rates due to changes in obstetrical factors, maternal medical conditions, or maternal mortality surveillance? Am J Obstet Gynecol 2024; https://doi.org/10.1016/j.ajog.2023.12.038(opens in new tab/window).
Roberto Romero, MD, DMedSci, Editor-in-Chief for Obstetrics of the American Journal of Obstetrics & Gynecology (AJOG), and Chief of the Pregnancy Research Branch of NICHD, NIH, stated, “Accurate assessment of the number and causes of maternal death is an important priority for countries and healthcare policymakers. Improving maternal mortality surveillance is key to formulating plans to improve maternal health. Comparisons of the rate of maternal death among countries should be interpreted with great caution because the methods of surveillance and accuracy differ. The article by Dr. Joseph and a distinguished group of epidemiologists and obstetricians published in AJOG calls attention to the need to improve surveillance in the United States and to thoughtful interpretation of reported statistics.”
Co-author Justin S. Brandt, MD, Director of the Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, NYU Grossman School of Medicine, notes, “By not relying on the pregnancy checkbox, our approach avoided the misclassification that has given the false impression of increasing maternal mortality rates in the US. Identifying maternal deaths by requiring mention of pregnancy among the multiple causes of death shows stable maternal mortality rates and declines in maternal deaths from direct obstetric causes.”
The research team previously published a study on maternal mortality in the US in 2017, which also showed stable rates of maternal mortality from 1999 to 2014. As mentioned, their results were subsequently validated by a detailed investigation carried out by the NCHS and published in January 2020.
Although the study’s findings contradict the mainstream narrative of high and rising rates of maternal death in the US, the results are consistent with changes in maternal characteristics and improvements in obstetric practice. For instance, the increase in maternal deaths due to specific placental complications (i.e., placenta accreta spectrum disorder) observed in their study is consistent with increases in deliveries to women with a previous cesarean delivery. Similarly, the reduction in maternal deaths due to hypertensive disorders in pregnancy (i.e., preeclampsia/eclampsia), blood clot embolism (i.e., thromboembolism), and infection (i.e., puerperal sepsis) is consistent with advances in the obstetric management of these conditions.
The study also showed a reduction in overall maternal mortality, and especially in maternal deaths from direct obstetric causes among non-Hispanic Blacks, which is encouraging. However, the disproportionately high rate of maternal death among Non-Hispanic Blacks in 2018–21 and the persistent racial/ethnic disparities are concerning, as is the small increase in direct obstetric deaths among non-Hispanic Whites.
Co-author Cande Ananth, PhD, MPH, MD, Division of Epidemiology and Biostatistics, Department of Obstetrics, Gynecology, and Reproductive Sciences; Cardiovascular Institute of New Jersey and Department of Medicine; and Environmental and Occupational Health Sciences Institute, Rutgers, Robert Wood Johnson Medical School; and Department of Biostatistics and Epidemiology, Rutgers School of Public Health, elaborates, “Our analysis suggests that people who are Black remain at much higher risk of dying due to pregnancy complications compared with people who are White. The continuing disparities in maternal mortality rates are concerning and deserve strategic and focused efforts to combat structural racism and designed to address chronic conditions disproportionately represented in this subpopulation.”
The study provides important insights into cause- and race/ethnicity-specific maternal mortality and provides suggestions for the appropriate use of the pregnancy checkbox on death certificates. The authors hope that these findings will serve as the evidentiary basis for clinical and public health initiatives for reducing maternal mortality.
Notes for editors
The article is “Maternal mortality in the United States: are the high and rising rates due to changes in obstetrical factors, maternal medical conditions, or maternal mortality surveillance?” by K.S. Joseph, MD, PhD; Sarka Lisonkova, MD, PhD; Amélie Boutin, MSc, PhD; Giulia M. Muraca, MPH, PhD; Neda Razaz, MPH, PhD; Sid John, MSc; Yasser Sabr, MHSc, MD; Wee-Shian Chan, MSc, MD; Azar Mehrabadi, MSc, PhD; Justin S. Brandt, MD; Enrique F. Schisterman, PhD; and Cande V. Ananth PhD, MPH (https://doi.org/10.1016/j.ajog.2023.12.038(opens in new tab/window)).It appears online ahead of volume 230, issue 4 of the American Journal of Obstetrics & Gynecology, published by Elsevier.
The article is freely available at https://www.ajog.org/article/S0002-9378(24)00005-X/fulltext(opens in new tab/window). To view the accompanying video, go to https://www.ajog.org/topic/ha-do-taxonomy/ha-video-ymob-ajogpresents(opens in new tab/window).
Full text of the article is also available to credentialed journalists upon request. Contact Andrea Boccelli, Senior Publisher, Elsevier, at +1 267 738 0357 or [email protected](opens in new tab/window) to obtain copies. To speak with the authors, please contact K.S. Joseph, MD, PhD, at [email protected](opens in new tab/window).
About the American Journal of Obstetrics & Gynecology
The American Journal of Obstetrics & Gynecology, “The Gray Journal,” covers the full spectrum of Obstetrics and Gynecology. The aim of the Journal is to publish original research (clinical and translational), reviews, opinions, video clips, podcasts and interviews that will have an impact on the understanding of health and disease and that has the potential to change the practice of women's health care. An important focus is the diagnosis, treatment, prediction, and prevention of obstetrical and gynecological disorders. The Journal also publishes work on the biology of reproduction, and content which provides insight into the physiology and mechanisms of obstetrical and gynecological diseases. It is the Official journal of the Society for Maternal-Fetal Medicine and the Infectious Diseases Society for Obstetrics and Gynecology. www.AJOG.org(opens in new tab/window)
About Elsevier
As a global leader in scientific information and analytics, Elsevier helps researchers and healthcare professionals advance science and improve health outcomes for the benefit of society. We do this by facilitating insights and critical decision-making with innovative solutions based on trusted, evidence-based content and advanced AI-enabled digital technologies.
We have supported the work of our research and healthcare communities for more than 140 years. Our 9,500 employees around the world, including 2,500 technologists, are dedicated to supporting researchers, librarians, academic leaders, funders, governments, R&D-intensive companies, doctors, nurses, future healthcare professionals and educators in their critical work. Our 2,900 scientific journals and iconic reference books include the foremost titles in their fields, including Cell Press, The Lancet and Gray’s Anatomy.
Together with the Elsevier Foundation(opens in new tab/window), we work in partnership with the communities we serve to advance inclusion and diversity in science, research and healthcare in developing countries and around the world.
Elsevier is part of RELX(opens in new tab/window), a global provider of information-based analytics and decision tools for professional and business customers. For more information on our work, digital solutions and content, visit www.elsevier.com.
Contact
AB