Quick Facts
Location: Abdominal cavity.
Arterial Supply: Branches of the superior and inferior mesenteric arteries (ileocolic, right colic, middle colic, left colic, sigmoid, and superior rectal arteries, respectively); the distal end is supplies by branches of the internal iliac artery (middle and inferior rectal arteries).
Venous Drainage: Ileocolic, right colic, middle colic, left colic, sigmoidal, superior rectal, middle rectal, and inferior rectal veins.
Innervation: Parasympathetic: vagus nerve (CN X), pelvic splanchnic nerves (S2-S4); Sympathetic: superior mesenteric plexus, superior and inferior hypogastric plexus, iliac plexus; Visceral afferents: spinal ganglia of L2-L3 or S1-S2; Enteric innervation.
Lymphatic Drainage: Superior and inferior mesenteric lymph nodes.
Related parts of the anatomy
Structure/Morphology
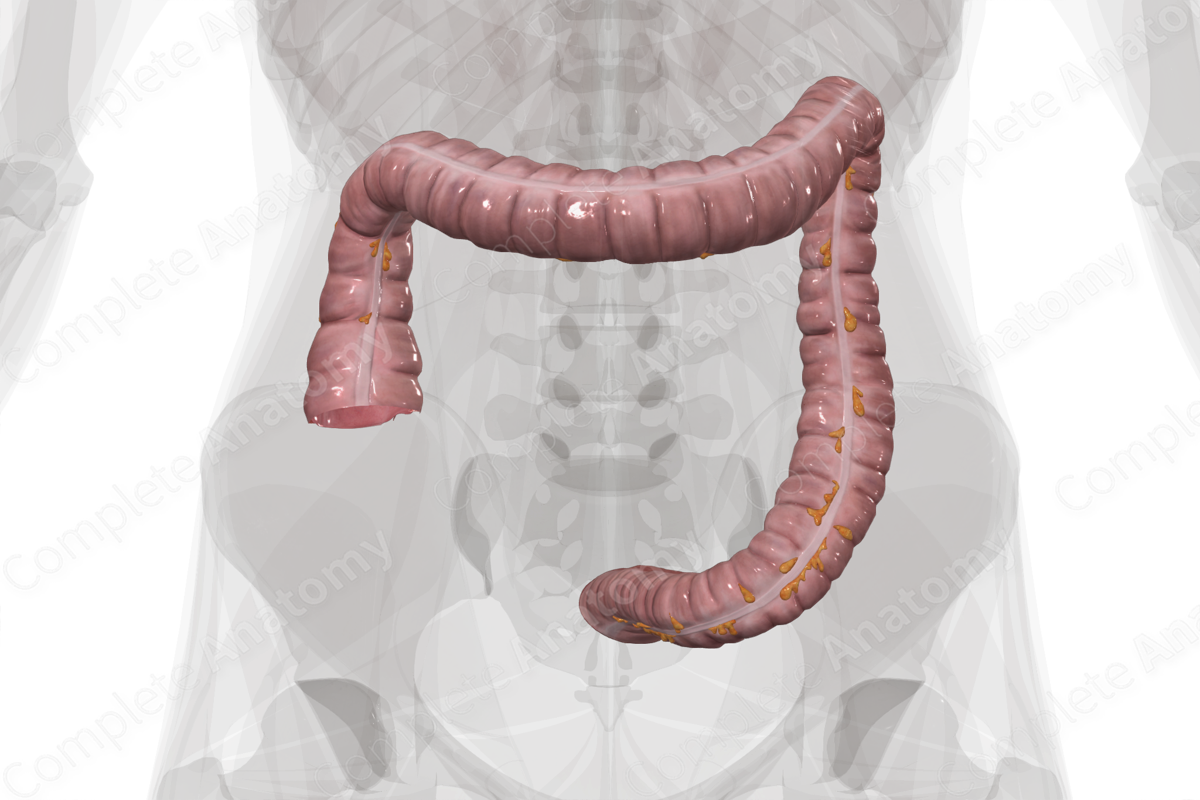
The colon is made up of four primary segments: ascending, transverse, descending, and sigmoid colon.
The cross-sectional microarchitecture of the large intestine demonstrates mucosa, submucosa, and muscularis (inner circular and outer longitudinal) layers with a thin outer serosal covering (Standring, 2016).
The longitudinal muscle arrangement of the cecum and colon is distinct. It contains three muscular bands called teniae coli. When the teniae coli contract, the colon is shortened leading to localized regions of expansion and constriction. These sacculations of the colon are called haustra. Between the haustra are the semilunar folds. These promote churning of chyme and increase the surface area of mucosa for absorption (Standring, 2016). These features are only found in the large intestine so are helpful in recognizing the colon in imaging. Additionally, small pockets of fat called the omental appendices project from the external (non-mesenteric) surface of most of the large intestine.
The ascending colon and proximal two thirds of the transverse colon are components of the midgut, while the remaining distal third is part of the hindgut. This developmental distinction is important in understanding the patterns of vascularization, innervation, and lymphatic drainage of the large intestine.
Anatomical Relations
Superior to the ileocecal junction is the ascending colon. It is secondarily retroperitoneal. Where the lateral border of the ascending colon lies in contact with the posterior abdominal wall, a small recess is formed called the right lateral paracolic gutter. A less distinct right medial paracolic gutter is present at the lateral margin, beyond which lie the small intestines. The ascending colon extends superiorly to the level of the right kidney where it variably lies ventral to its anterior surface. Further ascension is blocked by the inferior surface of the liver (approximately level of ninth and tenth rib), and, as a result, it makes a sharp bend to the left as the hepatic or right colic flexure (Standring, 2016).
At the hepatic flexure, the colon transitions to its transverse subdivision. The transverse colon arcs inferiorly from right to left across the abdominal cavity. It is intraperitoneal and is held in place by the transverse mesocolon. It continues as far as the hilum of the spleen ending at the splenic flexure. Here, the colon is anchored to the diaphragm by the phrenicocolic ligament.
The descending colon begins at the splenic flexure. It continues inferiorly, passing anterior to the left kidney. The small intestines lie medially, while the left lateral paracolic gutter lies laterally. The descending colon extends as far as the lesser pelvis where it becomes the sigmoid colon. The sigmoid colon continues medially, posteriorly and inferiorly into the true pelvis. On this course it crosses several structures including, from lateral to medial, the external and internal iliac vessels, the obturator nerve and the left ureter.
Function
The colon absorbs water, salts, vitamins, and minerals from the waste material. As a result, as it passes through the colon it becomes more and more solid. The colon contains a significant proportion of gastrointestinal bacteria which aids in the formation of feces and in the synthesis of essential vitamins (Koeppen and Stanton, 2009).
Arterial Supply
The colon is supplied by three colic branches of the superior mesenteric artery (Standring, 2016).
- The ileocolic artery supplies the ileocecal junction, cecum, and proximal ascending colon.
- The right colic artery supplies the mid-ascending colon to the hepatic flexure.
- The middle colic artery supplies from the hepatic flexure as far as the one half to two thirds of the transverse colon.
Similarly, the inferior mesenteric artery has three “sets” of branches (Standring, 2016).
- The left colic artery supplies the distal half to one third of the transverse colon and the descending colon.
- Usually two to three sigmoid arteries supply the sigmoid colon.
- The rectum is supplied by the superior, middle, and inferior anorectal arteries that are branches originating from the inferior mesenteric and internal iliac arteries, respectively.
It should be noted that the vascular territories of the colon and rectum overlap with that of adjacent arteries producing a significant anastomotic arterial “circle” often referred to as the marginal artery of the colon (of Drummond).
Venous Drainage
The venous drainage is into the portal circulation. The pattern largely parallels the arterial supply. The nutrient rich blood from superior and inferior mesenteric veins unite with the splenic vein forming the portal vein that drains into the liver.
Innervation
Innervation of the colon includes the enteric nervous system (sensory and motor), the autonomic nervous system (sympathetic and parasympathetic), as well as extrinsic sensory innervation (visceral afferents) (Standring, 2016).
The vagus nerve (CN X) provides parasympathetic innervation to the midgut components of the large intestine (ileocecal junction as far as the proximal two thirds of the transverse colon). The remainder of the large intestine receives parasympathetic innervation from the pelvic splanchnic nerves (S2-S4).
Sympathetic innervation is derived from the sympathetic chain or the aortic plexus. The proximal portion of the large intestine (as far as the proximal two thirds of the transverse colon), that is part of the midgut, is supplied by postganglionic neurons from the superior mesenteric plexus. The remainder of the large intestine, hindgut, is supplied by the inferior mesenteric, superior and inferior hypogastric plexuses. In addition, the iliac plexus and hypogastric nerve may contribute to the innervation of the sigmoid colon.
Visceral afferent nerves from the midgut ascend in tandem with the vagus nerve. In the hindgut the cell bodies of the visceral afferents reside in the spinal ganglia of L2-L3 or S1-S2.
The enteric system consists of two plexuses of densely packed small neurons. Meissner’s plexus lies in the submucosal layer and Auerbach’s myenteric plexus lie between the outer longitudinal and inner circular smooth muscle layers. These systems of nerves control mucosal and peristaltic function.
Lymphatic Drainage
Lymphatic drainage from the midgut component of the large intestine parallels the arterial supply and drain into superior mesenteric lymph nodes. In the hindgut, lymphatic drainage also follows arterial supply and drains into nodes along the inferior mesenteric artery via the inferior mesenteric lymph nodes (Földi et al., 2012).
List of Clinical Correlates
- Appendicitis
- Appendectomy
- Colitis
- Colonoscopy
- Crohn’s disease
- Diverticulitis
- Volvulus of the sigmoid colon
References
Földi, M., Földi, E., Strößenreuther, R. and Kubik, S. (2012) Földi's Textbook of Lymphology: for Physicians and Lymphedema Therapists. Elsevier Health Sciences.
Koeppen, B. M. and Stanton, B. A. (2009) Berne & Levy Physiology, Updated Edition E-Book. Elsevier Health Sciences.
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41st edn.: Elsevier Limited.
Learn more about this topic from other Elsevier products
Colon histology: Video, Causes, & Meaning

Colon histology: Symptoms, Causes, Videos & Quizzes | Learn Fast for Better Retention!
Colon

The colon is the final section of the gastrointestinal tract that extends from the cecum to the anal canal.




