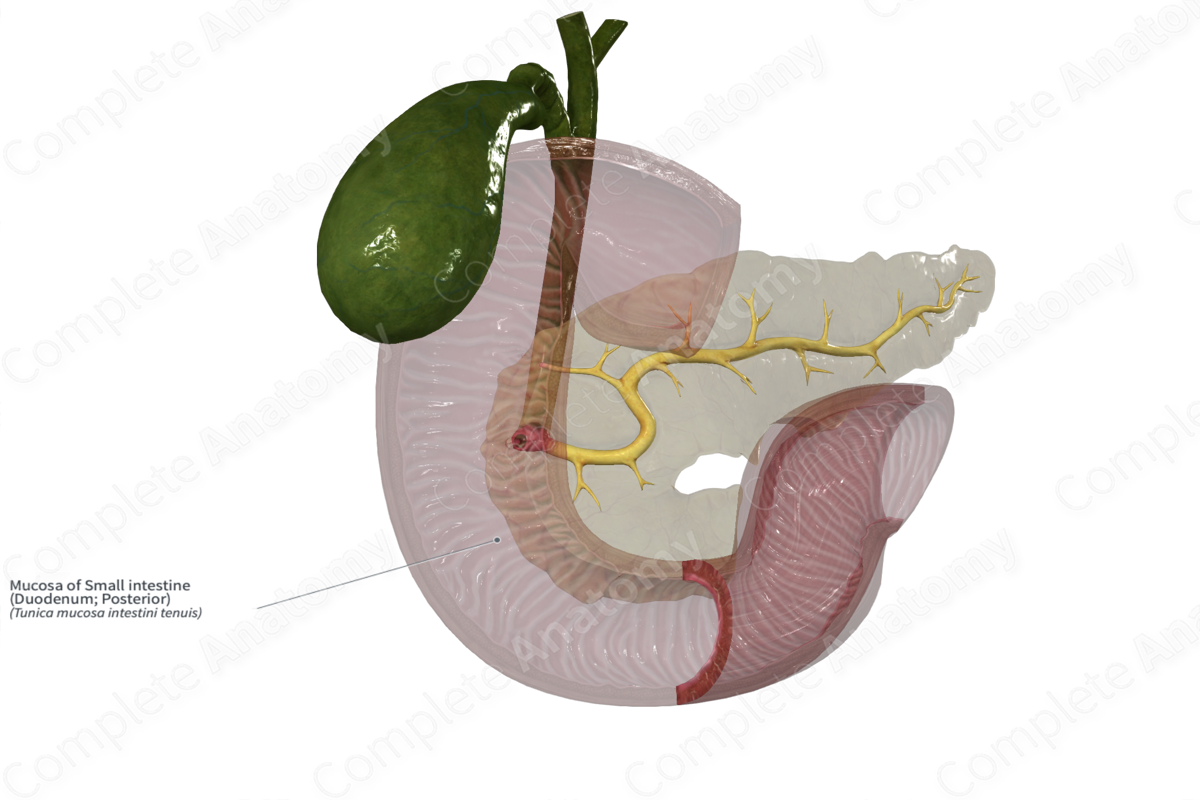
Mucosa of Small intestine (Duodenum; Posterior)
Tunica mucosa intestini tenuis
Read moreStructure/Morphology
The mucosa of the small intestine is the inner layer lining the duodenum, jejunum, and ileum. It consists of the epithelial layer that is in direct contact with the lumen, the lamina propria (loose connective tissue), and the muscularis mucosa, a thin layer of smooth muscle that marks the boundary with the submucosa.
Villi and microvilli are protrusions of the mucosa that increase the surface area to allow better absorption. These villi are separated by pits, called crypts. Stem cells are found within the crypts and are responsible for constantly replenishing the epithelial lining (Standring, 2016).
Related parts of the anatomy
Key Features/Anatomical Relations
The mucosa of the small intestine is the inner layer lining the duodenum, jejunum, and ileum. It's heavily involuted, with extensions called villi and depressions called crypts.
Brunner’s glands are found in the mucosa of the duodenum. Peyer’s patches in contrast are only found in the mucosa of the ileum.
Function
The mucosa of the small intestine is the major site of nutrient absorption.
Mucus secretions in the duodenum help neutralize the acidity of chyme as it enters from the stomach. Goblet cells found in the mucosa of the entire small intestine also produce mucus for lubrication.
Enterocytes (or absorptive cells) form the lining of the small intestine epithelium. These cells with their apical microvilli are the site at which nutrients are absorbed as well as sites at which final digestion of nutrients occurs (Standring, 2016).
List of Clinical Correlates
- Celiac disease
- Crohn’s disease
- Diarrhea
- Inflammatory bowel disease
References
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41 edn.: Elsevier Limited.
Learn more about this topic from other Elsevier products
Small Intestine Mucosa

The SI mucosa performs the intestinal barrier and absorptive functions, and is comprised of an intestinal epithelium covering the lamina propria that hosts the local mucosal immune system, and is surrounded by the submucosa and the outer muscle layers.




