Quick Facts
Location: Abdominal cavity.
Arterial Supply: Ileocolic artery, branch of the superior mesenteric artery.
Venous Drainage: Ileocolic vein, draining to the superior mesenteric vein.
Innervation: Parasympathetic: vagus nerve (CN X); Sympathetic: celiac ganglia; Visceral afferents: spinal ganglia of T5-T9; Enteric innervation.
Lymphatic Drainage: Peyer’s patches, ileocolic nodes, to the central superior mesenteric lymph nodes.
Structure/Morphology
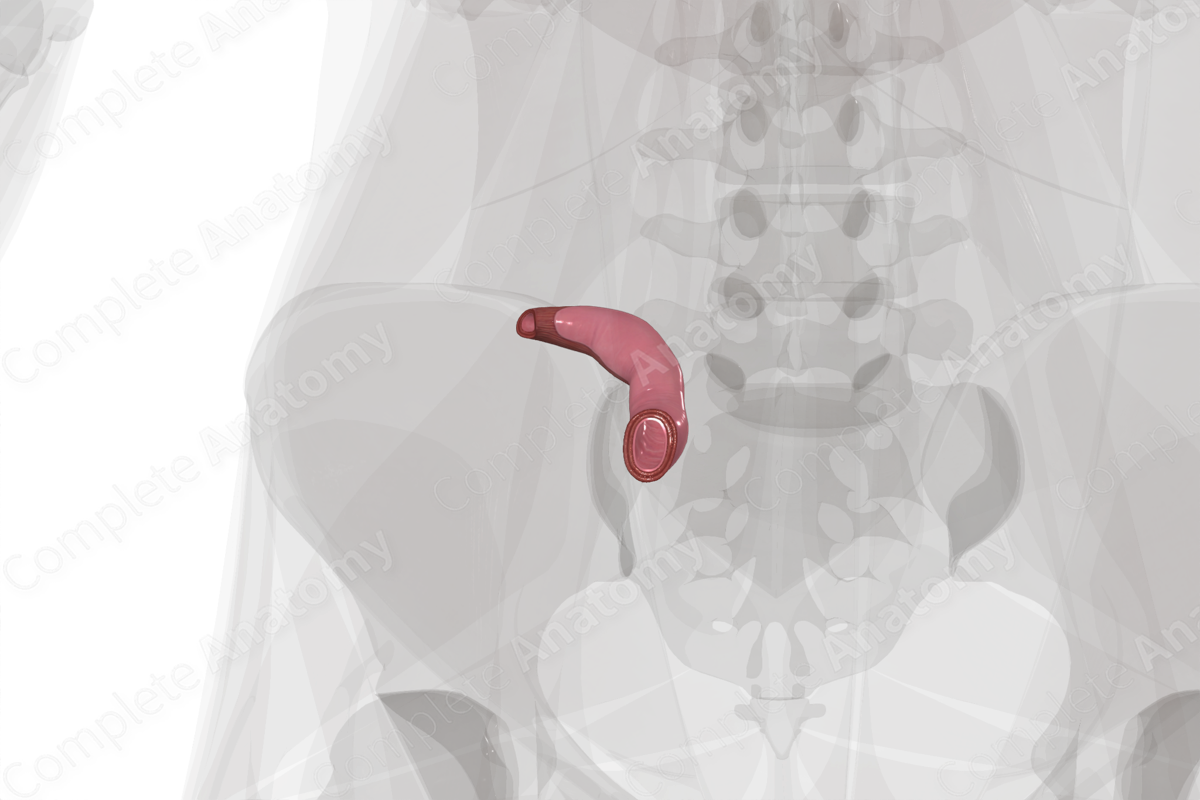
The terminal ileum is the final portion of the ileum and marks the end of the small intestine. The lumen of the terminal ileum is the site at which non-absorbed materials wait to be pushed through the ileocecal valve and into the large intestine.
The cross-sectional microarchitecture of the terminal ileum demonstrates mucosa, submucosa, and muscular (inner circular and outer longitudinal) layers with a thin outer serosal covering (Standring, 2016). The terminal ileum has fewer and smaller circular folds and villi than the jejunum, and a thinner mucosa. Brunner’s glands are absent and aggregated lymphoid nodules (Peyer’s patches) are abundant.
Anatomical Relations
The terminal ileum is the final part of the small intestine. It is intraperitoneal and sits in the lower right quadrant of the abdominal cavity, just medial to the cecum. The terminal ileum is attached to the posterior abdominal wall by the mesentery that carries the superior mesenteric vasculature. It ends at the ileal orifice, or ileocecal valve, through which chyme is sent to the cecum and large intestine.
Function
The terminal ileum is a site of absorption. It is also thought of as the spot where chyme is stored until the ileal orifice opens and allows it to pass into the large intestine (Standring, 2016).
Arterial Supply
The terminal ileum is supplied by ileal branches of the ileocolic artery, a major branch of the superior mesenteric artery.
Venous Drainage
The venous drainage is to the portal circulation. The pattern largely parallels the arterial supply.
Nutrient rich blood draining from the terminal ileum drains back through ileocolic vein, into the superior mesenteric vein, and into the portal vein and liver.
Innervation
Innervation of the terminal ileum includes the enteric nervous system (sensory and motor), the autonomic nervous system (sympathetic and parasympathetic), and extrinsic sensory innervation (visceral afferents) (Standring, 2016).
The vagus nerve (CNX) provides parasympathetic innervation to the terminal ileum.
Sympathetic innervation originates in the T5-T9 spinal cord levels with preganglionic neurons. The terminal ileum is supplied by postganglionic neurons from the celiac plexus and superior mesenteric plexus.
Visceral afferent nerves from the terminal ileum ascend along the vagus nerve or greater splanchnic nerve.
The enteric system consists of two plexuses of densely packed small neurons. Meissner’s plexus lies in the submucosal layer and Auerbach’s myenteric plexus lie between the outer longitudinal and inner circular smooth muscle layers. These systems of nerves control mucosal and peristaltic function.
Lymphatic Drainage
Lymph from the terminal ileum and its aggregated lymphoid nodules (or Peyer’s patches), drains from appendicular and ileocolic nodes into mesenteric nodes (Földi et al., 2012). From there, lymph drains into the central superior mesenteric nodes and ultimately to the cisterna chyli.
List of Clinical Correlates
- Crohn’s disease
- Terminal ileitis
References
Földi, M., Földi, E., Strößenreuther, R. and Kubik, S. (2012) Földi's Textbook of Lymphology: for Physicians and Lymphedema Therapists. Elsevier Health Sciences.
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41 edn.: Elsevier Limited.
Learn more about this topic from other Elsevier products
Terminal Ileum

The terminal ileum is identified as a loop of the small bowel joining the cecum;




