Quick Facts
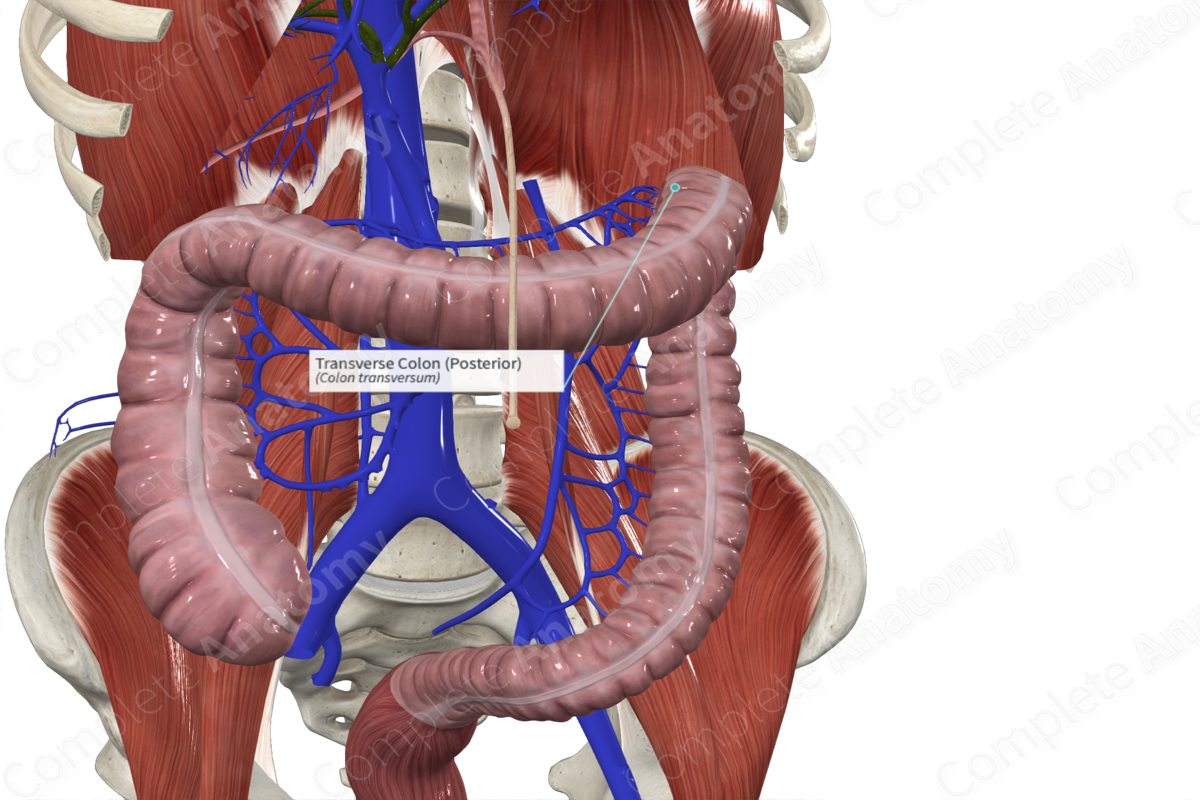
Location: Abdominal cavity.
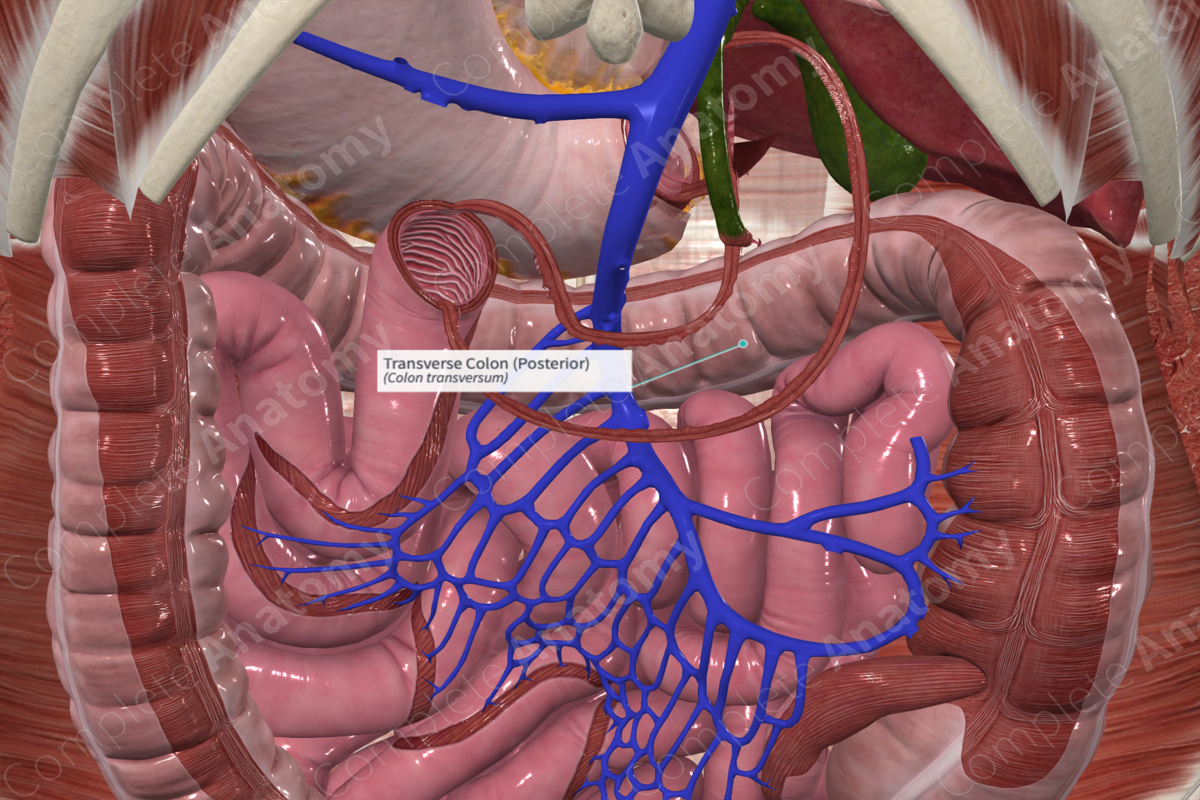
Arterial Supply: Middle colic artery (branch of the superior mesenteric artery) and left colic artery (branch of inferior mesenteric artery).
Venous Drainage: Middle and left colic veins.
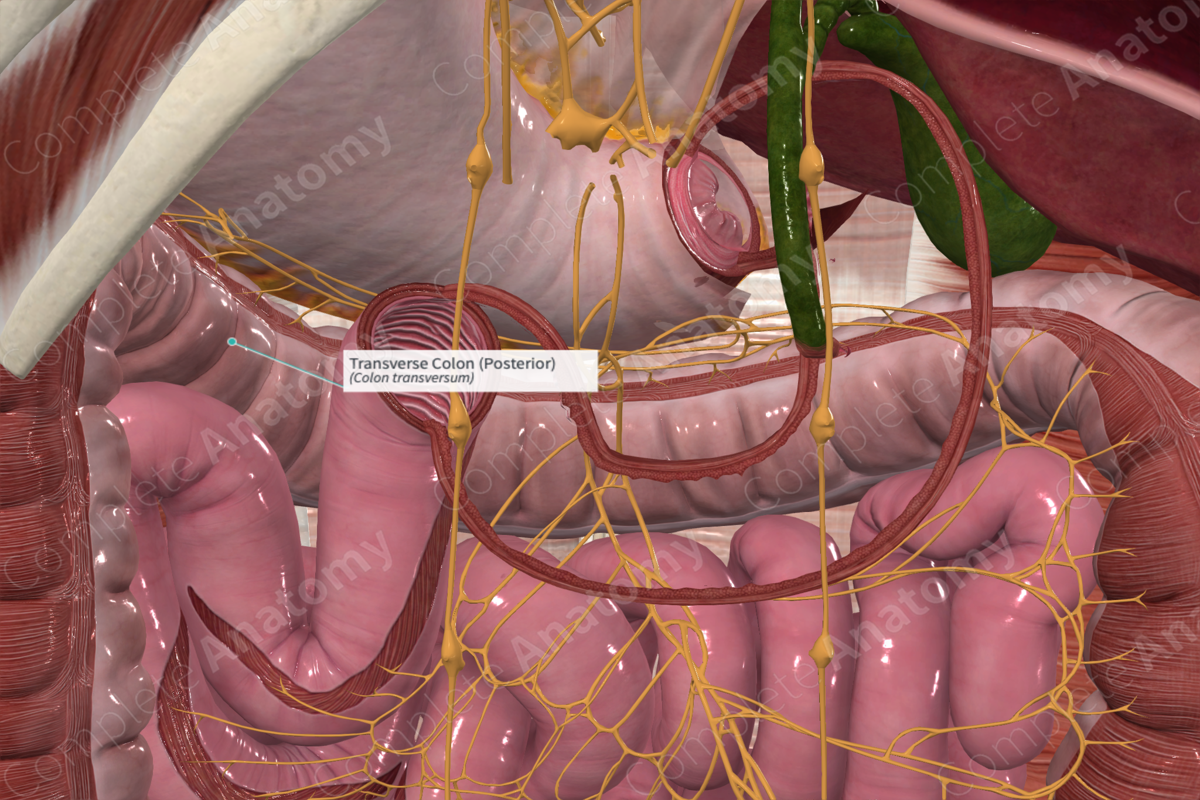
Innervation: Parasympathetic: vagus nerve (CN X) and pelvic splanchnic nerves (S2-S4); Sympathetic: superior and inferior mesenteric plexuses; Visceral afferents: T5-L2 spinal ganglia; Enteric innervation.
Lymphatic Drainage: Paracolic nodes to superior and inferior mesenteric lymph nodes.
Related parts of the anatomy
Structure/Morphology
The transverse colon is the portion of the large intestine between the hepatic and splenic flexures.
The cross-sectional microarchitecture of the transverse colon demonstrates mucosa, submucosa, and muscular (inner circular and outer longitudinal) layers with a thin outer serosal covering (Standring, 2016).
As with the rest of the large intestine, the longitudinal muscle arrangement of the transverse colon contains three muscular bands called teniae coli. Contraction of the teniae coli shortens the transverse colon to create sacculations or bulges called haustra. Between the haustra are the semilunar folds. These promote churning of chyme and increase the surface area of mucosa for absorption (Standring, 2016).
Additionally, small pockets of fat called the omental appendices project from the external (non-mesenteric) surface of most of the large intestine.
The transverse colon marks the boundary between midgut and hindgut, which helps explain the patterns of vascularization, innervation, and lymphatic drainage of this tissue. Typically, the proximal two thirds of the transverse colon is considered midgut and primarily supplied by superior mesenteric neurovasculature, while the distal third is considered hindgut and served primarily by inferior mesenteric neurovasculature.
Anatomical Relations
The transverse colon runs from the hepatic flexure proximally to the splenic flexure distally. It's intraperitoneal and held in place by the transverse mesocolon, a mesentery that connects it to the posterior abdominal wall. As it reaches the spleen, the transverse colon attaches to the diaphragm by the phrenicocolic ligament at the splenic flexure.
Function
The transverse colon absorbs water, salts, vitamins, and minerals from the waste material. As a result, as it passes through the colon it becomes more and more solid, with the contents of the ascending colon being more liquid than the rest. The colon contains a significant proportion of gastrointestinal bacteria which aids in the formation of feces and in the synthesis of essential vitamins (Koeppen and Stanton, 2009).
Arterial Supply
The transverse colon marks a watershed area where the tissue is supplied by different vasculature. The proximal two thirds are supplied by the middle colic artery, a branch of the superior mesenteric artery. The distal third is supplied by the left colic artery, a branch of the inferior mesenteric artery. The region where vascular supply transitions is susceptible to ischemia.
A significant anastomotic arterial “circle” known as the marginal artery of the colon (of Drummond) allows blood from an artery serving one area of the colon to pass to territories normally served by a different artery. In the transverse colon, this allows blood from the middle colic artery to serve distal transverse colon or blood from the left colic artery to serve proximal transverse colon.
Venous Drainage
The venous drainage is into the portal circulation. The pattern largely parallels the arterial supply, with blood from the middle colic vein draining into the superior mesenteric vein, then the portal vein, and finally into the liver.
Blood from the distal transverse colon drains from the left colic vein to the inferior mesenteric vein, the splenic vein, the portal vein, and into the liver.
Although oxygen poor, the venous blood from the transverse colon is nutrient rich.
Innervation
Innervation of the transverse colon includes the enteric nervous system (sensory and motor), the autonomic nervous system (sympathetic and parasympathetic), and extrinsic sensory innervation (visceral afferents) (Standring, 2016). Because the transverse colon includes both midgut and hindgut, the patterns of autonomic innervation are more complex than the rest of the large intestine.
The vagus nerve (CN X) provides parasympathetic innervation to the proximal two thirds of the transverse colon while pelvic splanchnic nerves from S2-S4 supply the distal third of the transverse colon.
Sympathetic innervation is derived from the sympathetic chain or the aortic plexus. The proximal two thirds of the transverse colon is supplied by postganglionic neurons from the celiac and superior mesenteric ganglia via the superior mesenteric plexus. The distal third of the transverse colon receives sympathetic neurons from the inferior mesenteric ganglia via the inferior mesenteric plexus.
Visceral afferent nerves from the transverse colon travel back to the CNS along the greater or lesser splanchnic nerves, the lumbar splanchnic nerves, or the vagus nerve.
The enteric system consists of two plexuses of densely packed small neurons. Meissner’s plexus lies in the submucosal layer and Auerbach’s myenteric plexus lie between the outer longitudinal and inner circular smooth muscle layers. These systems of nerves control mucosal and peristaltic function.
Lymphatic Drainage
Lymphatic drainage from the transverse colon parallels the arterial supply. Paracolic nodes drain into intermediate colic nodes, then to central superior mesenteric lymph nodes or the inferior mesenteric lymph nodes for the proximal two thirds or distal third of the transverse colon, respectively. Ultimately, all lymph is drained via the cisterna chyli and the thoracic lymphatic duct.
List of Clinical Correlates
- Colitis
- Colonoscopy
- Diverticulitis
- Colorectal Cancer
References
Koeppen, B. M. and Stanton, B. A. (2009) Berne & Levy Physiology, Updated Edition E-Book. Elsevier Health Sciences.
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41 edn.: Elsevier Limited.
Learn more about this topic from other Elsevier products