Quick Facts
Sympathetic Contribution: Greater thoracic splanchnic nerve.
Parasympathetic Contribution: Vagus nerve, anterior and posterior vagal trunks.
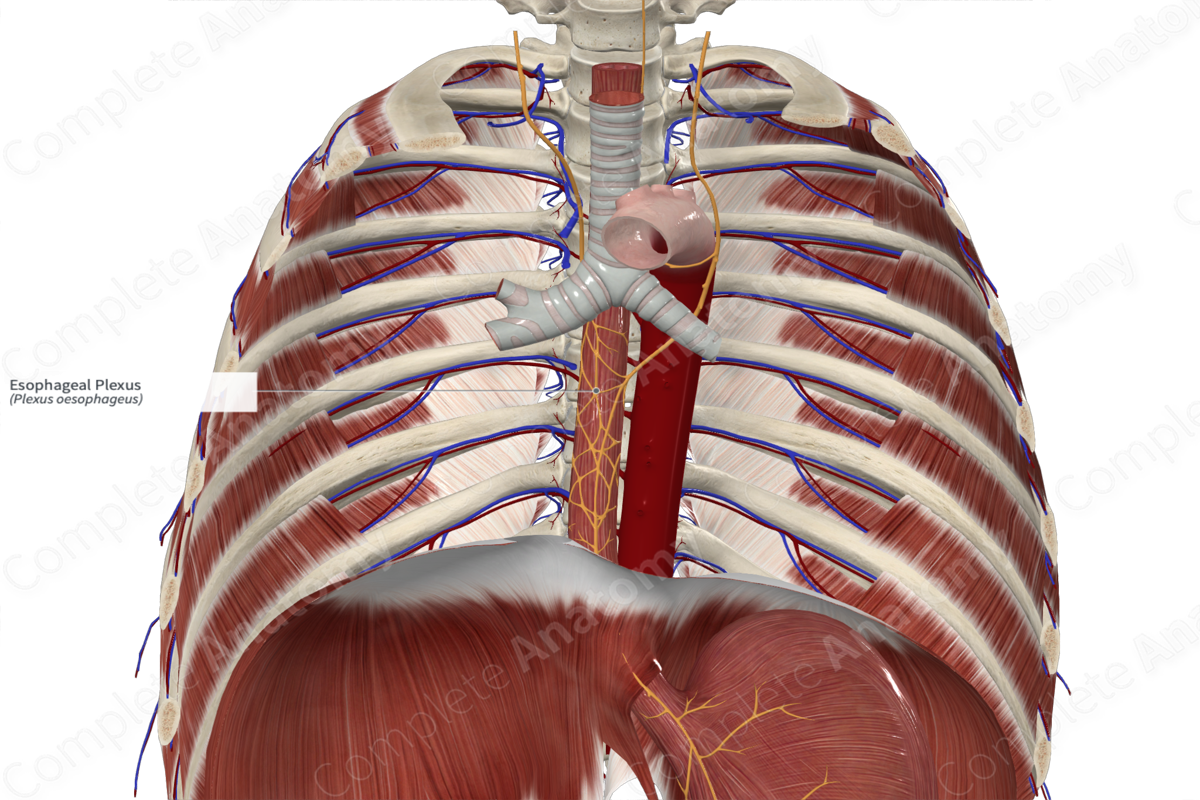
Course: Sits on the anterior and posterior surfaces of the esophagus from just below the cardiac plexus to the lower third of the esophagus.
Sympathetic Supply: Inhibition of esophageal smooth muscle.
Parasympathetic Supply: Contraction of striated and smooth muscle of the esophagus.
Contributing Nerves
The primary contribution to the esophageal plexus comes from the vagus nerve and fibers that originate in the posterior nucleus of the vagus nerve. The left vagus nerve fibers rotate to the anterior surface of the esophagus, forming much of the anterior esophageal plexus. The right vagus nerve ramifies into the posterior esophageal plexus on the posterior surface of the esophagus. The anterior and posterior esophageal plexuses give rise to the anterior and posterior vagal trunks, respectively.
The sympathetic component of the esophageal plexus comes from the thoracic sympathetic trunk, particularly from the ninth thoracic vertebral level and above (Netter, 2011). The cell bodies of their preganglionic sympathetic fibers are found in the intermediolateral cell columns of the thoracic segments of the spinal cord. The cell bodies of postganglionic neurons are found in thoracic sympathetic chain ganglia.
Course
The esophageal plexus is primarily composed of and best understood in the context of the vagus nerves. The left vagus nerve, just below the cardiac and pulmonary plexuses, ramifies into a plexus that rotates to the anterior surface of the esophagus. This forms much of the anterior esophageal plexus. The right vagus nerve ramifies into the posterior esophageal plexus which rotates to the posterior surface of the esophagus.
The anterior and posterior esophageal plexuses travel along their respective surfaces to the base of the thorax. They form back into two identifiable nerves, the anterior and posterior vagal trunks. These then pass through the diaphragm via the esophageal hiatus to enter the abdomen.
Branches
The esophageal plexuses condense back into two identifiable nerves towards the lower third of the thoracic esophagus. These are the anterior and posterior vagal trunks.
Supplied Structures & Function
The esophageal plexus supplies autonomic innervation to the mid and lower esophagus and transmits parasympathetic fibers to the abdomen. It is important to remember that as one descends in the esophagus, the enteric nervous system plays an increasingly important role, and the innervation and function of the sympathetic and parasympathetic systems become more complex and difficult to ascertain.
The cervical part of esophagus, which is primarily composed of striated muscle, receives inputs from the vagus nerve or recurrent laryngeal nerve and is superior to the formation of the esophageal plexus. Parasympathetic efferents to the esophageal plexus are generally associated with contraction of esophageal smooth muscle and rate of contraction. However, data indicates that parasympathetic fibers can regulate either inhibitory or excitatory enteric neurons in the esophageal wall (Corbin-Lewis and Liss, 2014). Parasympathetic vagal innervation of the esophageal plexus is also responsible for inhibition of the lower esophageal sphincter (Mittal, 2011). Additional parasympathetic effectors act on submucosal mucus glands in the esophageal wall, increasing the secretion of lubricants.
Sympathetic efferent fibers in the esophageal plexus regulate smooth muscle in arterial walls. Otherwise, they have an unclear role in the esophagus. Some sources claim little function, while others claim a role in tonic inhibition of esophageal smooth muscle and the lower esophageal sphincter (Zfass et al., 1970; Lyrenäs and Abrahamsson, 1986; Goyal and Chaudhury, 2008).
Visceral sensory afferents in the esophagus are associated with pain sensation and autonomic reflexes. The fibers associated with pain are thought to travel back to the spinal cord along the routes of sympathetic efferents. The autonomic reflexes associated with stretch are thought to travel back to the brainstem along the vagus nerve. It is possible some pain sensation also follows the vagus nerve back to the brainstem rather than the spinal cord.
List of Clinical Correlates
—Gastric reflux
—Dysphagia
References
Corbin-Lewis, K. and Liss, J. M. (2014) Clinical Anatomy & Physiology of the Swallow Mechanism. Cengage Learning.
Goyal, R. K. and Chaudhury, A. (2008) 'Physiology of normal esophageal motility', J Clin Gastroenterol, 42(5), pp. 610-9.
Lyrenäs, E. and Abrahamsson, H. (1986) 'Beta adrenergic influence on oesophageal peristalsis in man', Gut, 27(3), pp. 260-6.
Mittal, R. (2011) 'Motor Function of the Pharynx, Esophagus, and its Sphincters', in D. Neil Granger & ., J.P.G. (eds.) Integrated Systems Physiology: From Molecule to Function to Disease: Morgan & Claypool Life Sciences.
Netter, F. H. (2011) Atlas of Human Anatomy. Netter Basic Science Series: Saunders/Elsevier.
Zfass, A. M., Prince, R., Allen, F. N. and Farrar, J. T. (1970) 'Inhibitory beta adrenergic receptors in the human distal esophagus', Am J Dig Dis, 15(4), pp. 303-10.
Learn more about this topic from other Elsevier products





