Quick Facts
Sympathetic Contribution: Deep cardiac plexus.
Parasympathetic Contribution: Deep cardiac plexus.
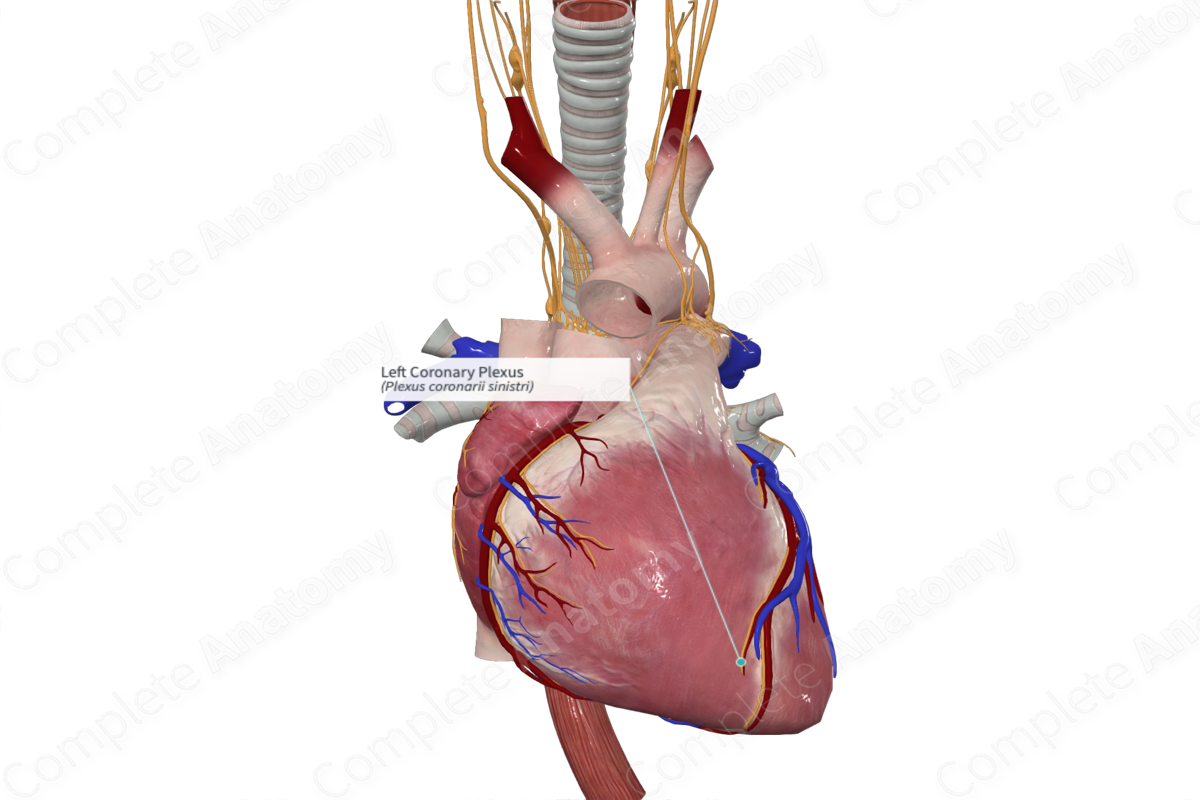
Course: From the deep cardiac plexus, running anteriorly along the left coronary artery, then spreading across the left side of the heart.
Sympathetic Supply: Increases heart rate, cardiac impulse conduction, and force of myocardial contraction, dilates coronary arteries.
Parasympathetic Supply: Decreases heart rate and force of myocardial contraction.
Contributing Nerves
The left coronary plexus is formed primarily from the deep cardiac plexus (Standring, 2016).
Course
The left coronary plexus runs anteriorly and follows the left coronary artery to reach the anterior surface of the heart after which it runs inferiorly supplying much of the left side of the heart (Standring, 2016).
Branches
The left coronary plexus has no named branches. Fibers leave the plexus to innervate surrounding cardiac tissue.
Supplied Structures & Function
The left coronary plexus provides both sympathetic and parasympathetic innervation to the heart, particularly the left side of the heart. Both types of nerve fibers pass from the plexus into the cardiac tissue by following the left coronary artery and its branches.
The sympathetic fibers lead to dilation of coronary arteries and increased rate and force of cardiac myofiber contraction. Parasympathetic fibers do the opposite, constricting coronary arteries and reducing heart rate.
Visceral sensory fibers traveling through the left coronary plexus convey information relating to pain, blood pressure, and blood chemistry back to the central nervous system.
List of Clinical Correlates
—Referred pain
References
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series: Elsevier Limited.
Learn more about this topic from other Elsevier products




