Quick Facts
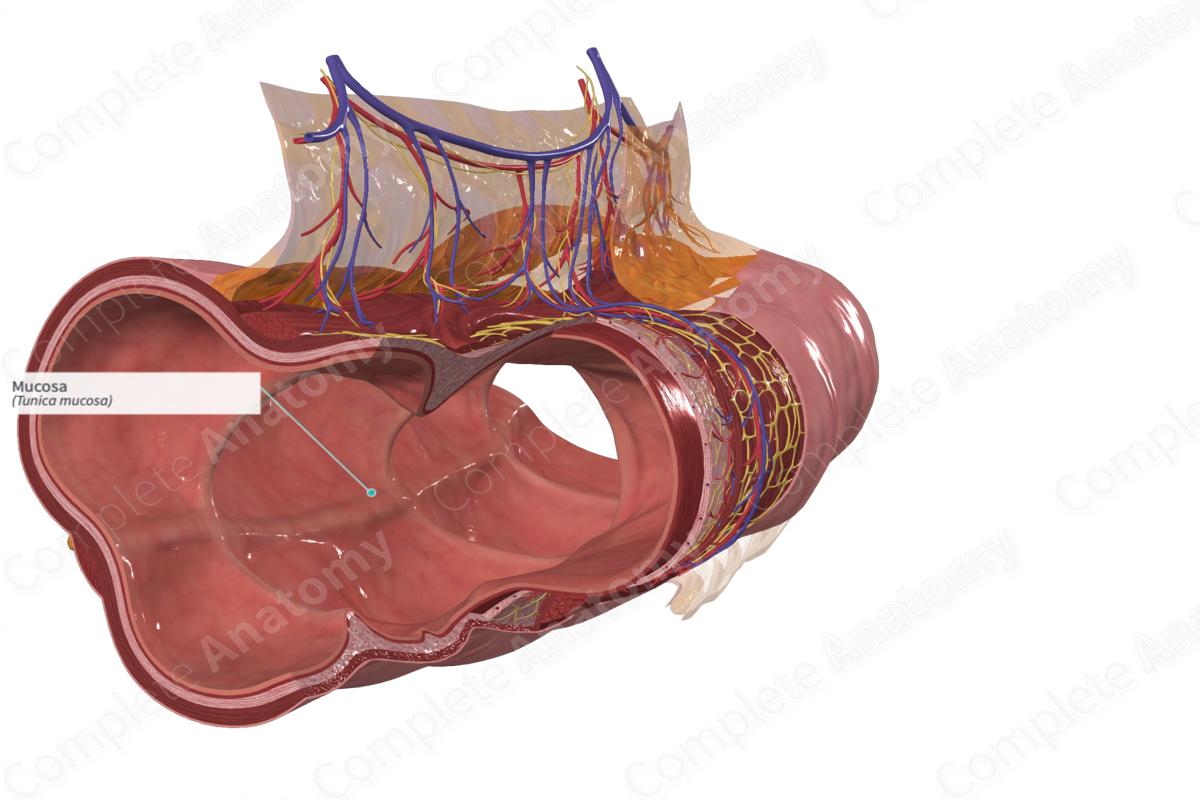
The mucosa is the mucous lining of various hollow structures, facing the lumen, comprising, in many locations, the epithelium, basement membrane, lamina propria mucosae, and lamina muscularis mucosae (Dorland, 2011).
Structure/Morphology
The mucosa lines the luminal surface of the large intestine and has a smooth, pale appearance. It consists of luminal surface epithelium, the lamina propria, and the muscularis mucosae (aids in the expulsion of intestinal crypt content/secretions particularly mucus secreted from goblet cells).
The luminal surface of the transverse colon is covered with simple columnar epithelium and goblet cells. The columnar cells have short microvilli located at the apex of their cell surface and tight cell junctions between the cells. The goblet cells are interspersed between the columnar cells. Intestinal crypts (or glands of Lieberkühn) are tubular pits of the mucosa and lie perpendicular to the lumen. They open directly into the lumen through small circular openings. The columnar epithelium extends into the crypts. Stem cells and neuroendocrine cells are also present in the crypts and are usually located near the base of the crypts (Standring, 2016). Stems cells continually divide to replace mucosal epithelial cells above them as they move towards the luminal surface and are shed several days later.
The mucosal regions adjacent to the lymphoid follicles contain microfold cells (M cells). These cells may be cuboidal or flattened and have widely spaced microfolds, rather than microvilli. They aim to take up foreign particles/antigens in the gut and pass them to the lymphoid tissue (Standring, 2016).
The lamina propria forms the intermediate layer between the epithelium and the muscularis mucosae and is made of loose connective tissue. It houses a diverse abundance of different cell types, such as connective tissue cells and immune cells, such as eosinophils, mast cells, and macrophages. It also contains capillaries, nerve fibers, and lymphatic vessels.
Anatomical Relations
The mucosa faces the gastrointestinal lumen and is in contact with its contents. It is superjacent to the muscularis mucosae and the submucosal layer.
Function
The mucosa provides a barrier-style protection against diffusion of unwanted particles or pathogens from the lumen to the internal tissues, as well as generating an immune response if the epithelial barrier is broken.
The columnar cells are involved in transepithelial transport functions and the tight junctions serve as a physical barrier that prevents diffusion of content from the gut lumen across the epithelial wall. The goblet cells secrete mucins, which forms and maintains the protective mucus blanket (Specian and Oliver, 1991). Microfold cells allow particle transport from the lumen to the lamina propria, where the immune cells can become involved.
In the intestinal crypts, the stem cells are capable of regenerating the different types of intestinal cells. They mitotically divide and provide cells which drift towards the intestinal luminal surface and primarily differentiate into columnar or goblet cells. The neuroendocrine cells secrete various chemokines and cytokines.
The lamina propria has two main roles. It provides structural support to the epithelium, forming part of the protective barrier separating pathogenic contact with the internal tissues. Additionally, due to its dense population of macrophages and lymphoid cells, it can generate effective immune responses if needed.
List of Clinical Correlates
—Crohn's disease
—Ulcerative Colitis
—Mucosa associated lymphoid tissue (MALT) lymphoma
References
Dorland, W. (2011) Dorland's Illustrated Medical Dictionary. 32nd edn. Philadelphia, USA: Elsevier Saunders.
Specian, R. D. and Oliver, M. G. (1991) 'Functional biology of intestinal goblet cells', Am J Physiol, 260(2 Pt 1), pp. C183-93.
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41st edition edn.: Elsevier Limited.
